by Womanaari | Sep 6, 2024 | Uncategorized
Understanding Vaginal Lumps: A Simple Guide
It is important to know that not all lumps cause concern. Vaginal lumps can vary in size, shape, and surface, ranging from not dangerous to serious ones. Figuring out the likely causes of side effects and when to look for medical help can assist you with dealing with your well-being with certainty.
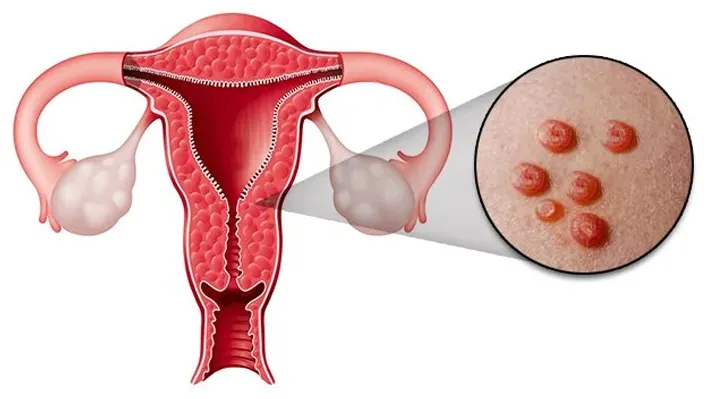
What is a Vaginal Lump?
Any visible bulge or growth that appears in or around the vaginal area is called a vaginal lump. These lumps can form on the vulva, the outer region of the female genitalia, or within the vaginal tract. They can be delicate or firm, easy or delicate, and sometimes be joined by side effects like tingling, agony, or discharge.
Common Causes of Vaginal Lumps
Various factors can cause vaginal lumps, a considerable lot of that are non-dangerous. Here are some causes:
• Bartholin’s Cyst: It is a liquid-filled lump close to the vaginal opening. It’s rarely serious but very well may be agonizing when infected.
• Inclusion Cysts: Small, harmless cysts that can shape on the walls of the vagina after a physical injury or surgery.
• Sebaceous Cysts: A small, slow-creating, non-cancerous lump filled with liquid or semi-liquid material that greases the skin and hair. These may show up on the vulva and are mostly harmless unless they become infected.
• Genital Warts: Soft growths that foster on genitals caused by the human papillomavirus. Despite the fact that they are painless, they are contagious and extremely agonizing occasionally.
• Abscesses: An abscess is a perplexing assortment of pus that can foster in the vaginal region because of infection, such as from a ruined Bartholin’s organ or an ingrown hair. Lessing the pus and pain consistently requires clinical treatment.
• Vaginal Varicosities: Vaginal varicosities, like varicose veins in the legs, have large veins that form as lumps in the vaginal region. These are often associated with pregnancy and, all around, resolve after delivery.
• Cancer: Usually uncommon, particular types of cancer, such as vulvar or vaginal cancer, can present as lumps in the vaginal region. These lumps are regularly firm and sporadic and might be joined by symptoms such as dying, tingling, or pain.
Symptoms to Watch For
While numerous vaginal lumps are harmless and not a cause for concern, it’s critical to know about specific symptoms that might show a more serious condition:
• Persistent pain: Assuming the lump is severe, and the pain does not subside, it might be a sign of an infection or abscess that needs clinical consideration.
• Rapid Development: A lump that grows rapidly or changes in appearance should be assessed medically.
• Unusual Discharge: Any unusual discharge, especially assuming it has a scent, maybe infection.
• Bleeding: Unexplained bleeding or spotting associated with a lump should be assessed by a specialist.
• Itching or Burning: These symptoms, especially if they persist, could be a sign of infection or other secret condition.
When to See a Doctor
If you notice a lump in your vagina, seek medical consultation if:
• The lump is painful, or enlarging or changing shape.
• Other symptoms appear, including fever, abnormal discharge, or bleeding.
• The lump persists for more than a few weeks.
• You have a medical history of cancer or other conditions that may heighten this risk.
When to go for Treatment
Early diagnosis and treatment can also prevent complications and ensure that any underlying issues are found and treated in time.
• Cyst and/or abscess: it may need to be drained, cleaned, put on antibiotics, and occasionally surgically excised if it is too large and/or apt to recur.
• Genital Warts: Medication treatments might be skin, cryotherapy (freezing), or surgical expulsion.
• Infections: Antibiotics or antifungal medications, much of the time, will be prescribed to treat lumps that are a result of a disease.
• Cancerous Lumps: The therapy for cancer lumps could be in the line of surgical activity, administration of radiation, or chemotherapy, contingent upon the sort and stage of the cancer.
Conclusion
Even though it very well might be very scary to find a lump in your vagina, most causes are usually harmless and treatable. By knowing the various causes and symptoms one will probably have, you can easily make purposeful strides in checking your well-being and knowing when to consult a physician. Regular check-ups and opening up with your healthcare provider remain highly instrumental in maintaining your vaginal health and concerns you might have. If you feel something weird, such as lumps or other symptoms, do not hesitate to consult your healthcare provider, who can provide a proper diagnosis and treatment.

by Womanaari | Sep 5, 2024 | Uncategorized
Grasping Cystocele: Causes, Side Effects, Medicines
A cystocele or a prolapsed bladder, is an ailment in which the wall between a female’s bladder and her vagina debilitates and broadens, letting the bladder to drop or lump into the vagina. It is many times the consequence of delivery, difficult work, or various sorts of strain that can weaken the pelvic muscles. It can go from gentle to serious but is a treatable condition.
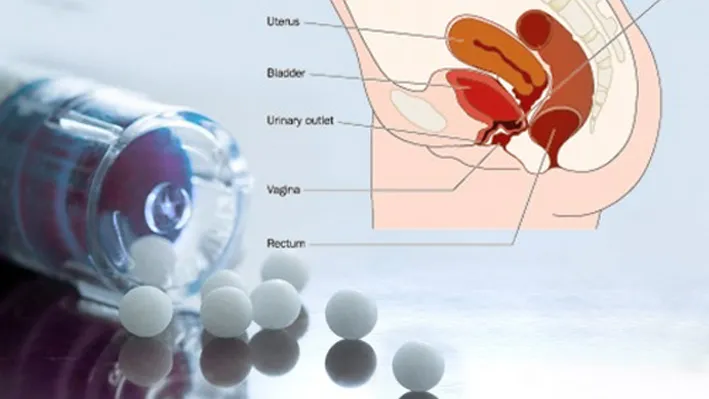
Meaning
A cystocele is a type of pelvic organ prolapse, where the bladder drops into the vaginal wall. This happens upon the weakening of the pelvic floor muscles and connective tissues that support the bladder. Contingent upon the seriousness, a cystocele is characterized into three grades:
Grade 1 (Gentle): The bladder drops simply a short way into the vagina.
Grade 2 (Moderate): The bladder has sunk far at the vaginal opening.
Grade 3 (Extreme): The bladder grows out through the vagina.
Causes
Cystocele frequently creates because of a mix of elements that debilitate the pelvic floor muscles. A portion of the essential drivers include:
Labor: Vaginal delivery, especially with troublesome or various births, can strain and damage the muscles and tissues supporting the bladder, provoking cystocele.
Menopause: The decrease in estrogen levels after menopause can cripple the pelvic floor, making it more leaned to prolapse.
Overweight: Overflow body weight adds additional strain to the pelvic floor, which can provoke cystocele after some time.
Persistent Straining: Conditions like ongoing bronchitis, or difficult work can come down on the pelvic floor, adding to the risk of cystocele.
Maturing: As ladies age, the muscles and tissues normally lose strength and flexibility, expanding the gamble of a prolapsed bladder.
Side effects
The side effects of cystocele can change dependent upon the earnestness of the prolapse. Ordinary side effects include:
• An impression of tension or strain in the pelvis or vagina.
• A knot in the vagina that may be recognizable or felt.
• Trouble emptying the bladder totally.
• Uneasiness during sex.
• Urinary incontinence, particularly during practices like hacking or working out.
Treatment
Pelvic Floor Activities: Otherwise called Kegel works out, these reinforce the pelvic muscles and can assist with reducing symptoms in mild cases.
Pessary: A pessary is a removable gadget embedded into the vagina to help the bladder and keep it set up. It very well may be an effective non-surgical choice for some ladies.
Way of life Changes: Weight reduction, abstaining from difficult work, and treating persistent coughing or blockage can lessen the stress on the pelvic floor and prevent deteriorating of the prolapse.
Colporrhaphy: This is a common procedure that fixes the tissue between the bladder and vagina, restoring the bladder to its normal position.
Minimally Intrusive Methodology: For less extreme cases, procedures like laparoscopic or robotic helped strategies can be performed to decrease recuperation time and complications.
When to Look for Medical Consultation
It’s vital to counsel a medical services supplier if you experience any of the symptoms related with cystocele, especially in the event that they are influencing your personal satisfaction. Early analysis and treatment can keep the condition from declining and work on in general solace and capability. Ladies who have as of late conceived, those going through menopause, or those with a background marked by pelvic floor problems ought to be especially watchful and look for clinical guidance on the off chance that they notice any symptoms of a prolapsed bladder.
Conclusion
Cystocele is a typical condition that can fundamentally influence a lady’s everyday existence, except it is sensible with proper care and treatment. By understanding the causes, perceiving the symptoms, and exploring treatment options, ladies can find proactive ways to address this condition. Early intervention with a medical care supplier is critical to tracking down the best arrangement and keeping up with pelvic wellbeing.

by Womanaari | Sep 5, 2024 | Uncategorized
Grasping Ovarian Cysts: A Manual Guide
Ovarian cysts are a typical issue that various women face in their lives. While “blister” can sound upsetting, it is fundamental to understand what ovarian cysts are, formation, and treatment. This guide will you figure out ovarian cysts, helping you with making informed choice about your prosperity.
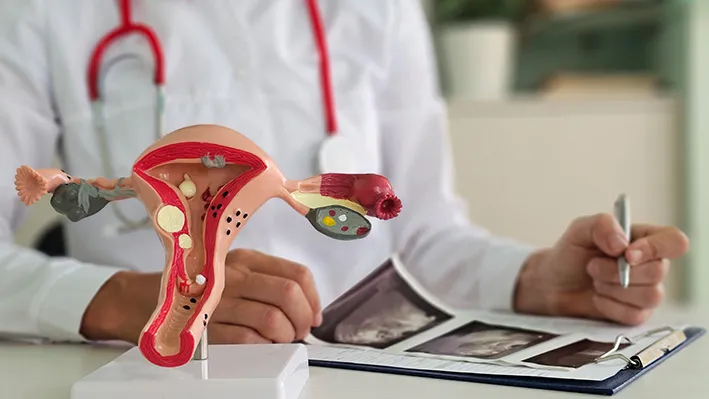
What Are Ovarian Cysts?
Ovarian cysts are fluid-filled sacs that can grow on or inside a female’s ovaries. The ovaries are vital for female reproduction, liable for producing eggs and hormones like estrogen and progesterone. These chemicals direct the monthly cycle and are important in pregnancy. Most ladies have two ovaries, one on each side of the uterus.
Cysts can shape in different ways and are very normal. As a matter of fact, numerous ladies will foster one during their lifetime, frequently without knowing it. Most ovarian cysts are innocuous and disappear all alone without bringing out any side effects. However, sometimes, cysts can become bigger and cause uneasiness or other medical problems.
Types
There are various ovarian cysts having different characteristics:
1. Functional Cysts. They are of two types: Follicular Cysts and Corpus Luteum Cysts
2. Dermoid Cysts
3. Endometriomas
4. Cystadenomas
5. Polycystic Ovaries
Symptoms
Ovarian cysts cause no side effects and are just found during routine pelvic exams or imaging tests. Nonetheless, bigger cysts or those that cause complexities might prompt observable side effects, including:
• Pelvic torment, which might be a dull hurt or a sharp torment, frequently on one side of the lower midsection
• Swelling or a sensation of fullness in the midsection
• Pain during intercourse
• Painful or irregular periods
• Urinary desperation or trouble emptying the bladder
• Nausea or vomiting
If you experience abrupt, extreme stomach torment, alongside side effects, for example, fever or vomiting, looking for guaranteed clinical attention is significant. These side effects could demonstrate a twisted or burst growth, which requires immediate treatment.
Diagnosing and Treatment
If your physician thinks that you have an ovarian growth, they might prescribe different tests to affirm the diagnosis and know its sort and size. Common diagnostic tests include:
• Ultrasound
• Blood Tests
The treatment for ovarian cysts relies upon the type, size, and side effects. Choices include:
1. Careful Waiting: In the event that the blister is little and not causing side effects, your doctor might propose checking it with ultrasounds to check whether it changes or disappears all alone.
2. Medicines: Contraception pills or other hormonal meds might be endorsed to assist with keeping new cysts from developing.
3. Medical procedure: Assuming the sore is huge, persistent, or causing critical side effects, your doctor might prescribe a medical procedure to eliminate it. This should frequently be possible utilizing a negligibly intrusive strategy called laparoscopy, which includes little cuts and a speedier recuperation time.
Preventing Ovarian Cysts
While there is no reliable method for forestalling ovarian cysts, regular pelvic tests can assist with getting them right on time before they cause complications. Overseeing fundamental circumstances like PCOS, endometriosis, and hormonal imbalances may likewise lessen your danger of creating cysts.
Conclusion
Ovarian cysts are a typical condition that most ladies will insight sooner or later in their lives. While they are frequently innocuous and disappear all alone, it’s critical to know about the side effects and look for clinical guidance assuming you have any worries. With proper checking and treatment, ovarian cysts can be actually handled, guaranteeing your general wellbeing and prosperity. Standard check-ups and remaining informed about your reproductive wellbeing are vital to forestalling and resolving any potential issues connected with ovarian cysts.

by Womanaari | Sep 5, 2024 | Uncategorized
Understanding Painful Periods (Dysmenorrhea): A Simple Guide
Dysmenorrhea, or painful periods, is a common problem for women. It is characterized by crampy lower midsection pain before or during a flow. While some women feel mild discomfort, others can experience extreme pain, which interferes with their usual activities. Knowing the cause, signs, and treatment associated with dysmenorrhea helps you cope better.
Dysmenorrhea is partitioned into two types:
Primary Dysmenorrhea: This is normal in young ladies and usually starts a little while after their first period. It stems from the usual contractions of the uterus, which is shedding its lining. The contractions are provoked by hormones called prostaglandins.
Secondary Dysmenorrhea: It results from built-up illnesses such as fibroids, endometriosis, or pelvic inflammatory disease. Pain starts much earlier in cycle and is present much more time; it even may increase after a definite period.
Causes of Painful Periods
The primary cause of dysmenorrhea is the compression of the uterus to remove its covering. In any case, certain factors can worsen the pain:
•High Levels of Prostaglandins: These chemical-like substances trigger uterine contractions, creating more intense cramps.
•Endometriosis: Tissues in the uterine membranous coating enlarge during menstruation.
•Fibroids: Harmless tumours that may lead to painful menstrual periods.
•Pelvic Inflammatory Disease (PID): Period pain will cause continued pelvic aches and swelling.
•Adenomyosis: This covering goes on extending up to the wall of the muscle and results in very severe contraction.
Symptoms of Dysmenorrhea
Although they can vary, dysmenorrhea symptoms usually consist of:
• Lower Abdominal Pain
• Nausea and Vomiting
• Headaches
• Fatigue
• Heavy Menstrual Flow
Diagnosis and Treatment
Talking with a doctor about your period history and symptoms is necessary to diagnose dysmenorrhea. Prescribing additional tests like ultrasound, MRI, and laparoscopy are useful in precluding covered conditions.
Treatment depends on the severity of the pain and the fundamental cause. Common options include:
• Over-the-Counter Pain Relievers
• Hormonal Birth Control Pills, patches, or IUDs
• Heat Therapy or Heating Pads
• Regular Exercise
• Dietary Changes
• Alternative therapies like acupuncture, yoga, and massage therapy
When to Consult a Doctor
While mild and moderate menstrual pains are pretty much normal, the severe pain is absolutely not and a professional health provider should assess for it. When your periods are so painful it makes it difficult to perform your day-to-day functions, heavy bleeding, irregular periods, or the pain intensifies over a long period, it’s vital to seek medical attention.
Conclusion
Painful periods, or dysmenorrhea, can be challenging, but they really do make sense with the right intervention. Knowing the tymptoms, their causes, and treatment options will help you take responsibility for your menstrual health. In case the pain becomes unbearable, then it would be wise to consult with a healthcare giver for more advice and support. It can only assist one to maintain a healthy lifestyle with proper management through the menstrual period.

by Womanaari | Sep 3, 2024 | Uncategorized
Understanding What Exactly is Menopause: Overview
Menopause is just a purely natural biologic event that describes the absence of a woman’s menstrual periods. It is an indication giving a cue to the end of a woman’s reproductive cycle. The process of menopause can be observed at any point in between the ages of 45 to 55 years; however, with some other women, it purely can take place at any age. It is generally defined as twelve consecutive months of no menstrual period. Menopause is anticipated by a woman for the natural phenomenon of the life cycle; but definitely, sentiments and emotions about it can trouble a woman. The knowledge of what menopause is, what type of symptoms to anticipate and how to tackle them can probably help make the transition much smoother over
Most women experience menopause when their ovaries reduce the production of the hormones estrogen and progesterone—both essential in controlling the menstrual cycle. When it reduces the levels of these hormones, the eggs are utilized slowly after which no eggs would remain which would stop the menstruation cycle. The period before menopause is referred to as perimenopause and usually is many years in most women where the levels of these hormones fluctuate and sometimes give up symptoms of menopause.
Menopause Symptoms
Though in the case of every woman, symptoms may vary, there are some typical symptoms. These typically include:
• Hot Flashes: They are characterized by unexpected increases in body temperature, a transient blood pressure, and a sweat potentially causing flushing of the face, neck, and chest. These types of flushes, according to statistics of their timing, durations, and even time of day they occur, last from 30 seconds to, on average, 10 minutes.
– Night Sweats: These can be considered the literal hot flash that is experienced at night, causing much sweat that it also messes up the woman’s pattern of sleep.
– Irregular Periods: In perimenopause, periods will find a way to be irregular. Some become longer or shorter, heavier or lighter, and eventually some just stop altogether.
• Vaginal Dryness: The vagina dries up, corresponding with decreasing doses of estrogen, and the vaginal tissues get thin. Sexual intercourse becomes painful, and the chances of a urinary tract infection increase.
• Mood Swings: Huge hormonal changes make a woman prone to mood swings, irritability, etc., which have more tendencies to bring about depression and anxiety.
• Sleep Disturbance: Most females in this age group report lacking sleep disorders caused by night sweats, insomnia, or other factors related to this.
• Weight Gain: Hormonal changes that occur during the perimenopausal period may lead to changed metabolism in women, tending to put on more weight, especially around the lower abdomen.
• Thinning Hair and Dry Skin: The hair begins to thin, and the skin starts to dry, becoming less supple.
Dealing with Menopause
While menopause is a natural fact of life, its symptoms can be very uncomfortable indeed and it can mean weeks of disruptions. The following ways can help you alleviate or control these symptoms:
• Hormone Replacement Therapy (HRT): This treatment affects the menopausal symptoms by giving women with estrogen and progesterone. Doing so could help alleviate problems such as hot flashes, sweating at night, or dryness in the vagina. However, it won’t suit everybody, so consult a doctor to know the risks weighed against the benefits of such treatment.
• Lifestyle factors: Regular exercise and healthy diet with maintenance of normal weight may be helpful in reducing weight gain, changes in mood and sleeping pattern. Reduction in alcohol and caffeine intake before bedtime can promote sound sleep. Activity keeps the mind busy and generates the capability of coping with stress.
• Stress management: Deep breathing, yoga, meditation, and mindfulness are some such activities. These in turn will help reduce your stress levels and enhance your mood. Some antidepressants and blood pressure drugs can be given to women who cannot take HRT to reduce side effects such as hot flashes. These are non-hormonal medications.
• Vaginal Moisturizers and Lubricants: If you face dryness during sex, then you may use various types of vaginal moisturizers or lubricants to make things a little more comfortable.
Baseline Health Screenings: As menopausal women are at high risk for several conditions such as osteoporosis and heart diseases, regular check-ups are necessary. In order to maintain health its is advised to have timely blood pressure and complete cholesterol level tests.
When to Consult a Doctor
Menopause is a natural course. The patient-based consultation with the health care professional should be sought only when the symptoms are severe or distressing. It constitutes,
• Heavy Bleeding: In case of heavy bleeding, that is far more than your normal period or lasts far longer than a normal period, that’s a reason to speak with a clinician.
•Severe Hot Flashes or Night Sweats: If hot flashes or night sweats are truly significantly disrupting your life, a health care professional can talk about possibilities—one of them being treatments.
Mood Changes: Should you feel overly depressed, anxious, or moody, by all means, schedule an appointment with your healthcare practitioner. Hormonal changes can exacerbate these feelings, but there is no need to suffer in silence.
Bone Health Concerns: If strong family history of osteoporosis or other bone density disorders — discuss with your physician to get bone density tested and how to get ahead of the ball on prevention.
Conclusion
Menopause is a unique life passage of changes that could occur, both physically and emotionally. That can be challenging, but the more informed a woman is with respect to what to expect and how to manage the symptoms, the easier the process becomes. With lifestyle adjustments and medical treatment or just being better informed, a woman becomes better equipped to handle menopause. Whatever concerns around menopause or its symptoms that may arise, never shy away from seeking advice and being supported by your health professional—always individually tailored to you.