by Womanaari | Sep 3, 2024 | Uncategorized
Understanding What Exactly is Menopause: Overview
Menopause is just a purely natural biologic event that describes the absence of a woman’s menstrual periods. It is an indication giving a cue to the end of a woman’s reproductive cycle. The process of menopause can be observed at any point in between the ages of 45 to 55 years; however, with some other women, it purely can take place at any age. It is generally defined as twelve consecutive months of no menstrual period. Menopause is anticipated by a woman for the natural phenomenon of the life cycle; but definitely, sentiments and emotions about it can trouble a woman. The knowledge of what menopause is, what type of symptoms to anticipate and how to tackle them can probably help make the transition much smoother over
Most women experience menopause when their ovaries reduce the production of the hormones estrogen and progesterone—both essential in controlling the menstrual cycle. When it reduces the levels of these hormones, the eggs are utilized slowly after which no eggs would remain which would stop the menstruation cycle. The period before menopause is referred to as perimenopause and usually is many years in most women where the levels of these hormones fluctuate and sometimes give up symptoms of menopause.
Menopause Symptoms
Though in the case of every woman, symptoms may vary, there are some typical symptoms. These typically include:
• Hot Flashes: They are characterized by unexpected increases in body temperature, a transient blood pressure, and a sweat potentially causing flushing of the face, neck, and chest. These types of flushes, according to statistics of their timing, durations, and even time of day they occur, last from 30 seconds to, on average, 10 minutes.
– Night Sweats: These can be considered the literal hot flash that is experienced at night, causing much sweat that it also messes up the woman’s pattern of sleep.
– Irregular Periods: In perimenopause, periods will find a way to be irregular. Some become longer or shorter, heavier or lighter, and eventually some just stop altogether.
• Vaginal Dryness: The vagina dries up, corresponding with decreasing doses of estrogen, and the vaginal tissues get thin. Sexual intercourse becomes painful, and the chances of a urinary tract infection increase.
• Mood Swings: Huge hormonal changes make a woman prone to mood swings, irritability, etc., which have more tendencies to bring about depression and anxiety.
• Sleep Disturbance: Most females in this age group report lacking sleep disorders caused by night sweats, insomnia, or other factors related to this.
• Weight Gain: Hormonal changes that occur during the perimenopausal period may lead to changed metabolism in women, tending to put on more weight, especially around the lower abdomen.
• Thinning Hair and Dry Skin: The hair begins to thin, and the skin starts to dry, becoming less supple.
Dealing with Menopause
While menopause is a natural fact of life, its symptoms can be very uncomfortable indeed and it can mean weeks of disruptions. The following ways can help you alleviate or control these symptoms:
• Hormone Replacement Therapy (HRT): This treatment affects the menopausal symptoms by giving women with estrogen and progesterone. Doing so could help alleviate problems such as hot flashes, sweating at night, or dryness in the vagina. However, it won’t suit everybody, so consult a doctor to know the risks weighed against the benefits of such treatment.
• Lifestyle factors: Regular exercise and healthy diet with maintenance of normal weight may be helpful in reducing weight gain, changes in mood and sleeping pattern. Reduction in alcohol and caffeine intake before bedtime can promote sound sleep. Activity keeps the mind busy and generates the capability of coping with stress.
• Stress management: Deep breathing, yoga, meditation, and mindfulness are some such activities. These in turn will help reduce your stress levels and enhance your mood. Some antidepressants and blood pressure drugs can be given to women who cannot take HRT to reduce side effects such as hot flashes. These are non-hormonal medications.
• Vaginal Moisturizers and Lubricants: If you face dryness during sex, then you may use various types of vaginal moisturizers or lubricants to make things a little more comfortable.
Baseline Health Screenings: As menopausal women are at high risk for several conditions such as osteoporosis and heart diseases, regular check-ups are necessary. In order to maintain health its is advised to have timely blood pressure and complete cholesterol level tests.
When to Consult a Doctor
Menopause is a natural course. The patient-based consultation with the health care professional should be sought only when the symptoms are severe or distressing. It constitutes,
• Heavy Bleeding: In case of heavy bleeding, that is far more than your normal period or lasts far longer than a normal period, that’s a reason to speak with a clinician.
•Severe Hot Flashes or Night Sweats: If hot flashes or night sweats are truly significantly disrupting your life, a health care professional can talk about possibilities—one of them being treatments.
Mood Changes: Should you feel overly depressed, anxious, or moody, by all means, schedule an appointment with your healthcare practitioner. Hormonal changes can exacerbate these feelings, but there is no need to suffer in silence.
Bone Health Concerns: If strong family history of osteoporosis or other bone density disorders — discuss with your physician to get bone density tested and how to get ahead of the ball on prevention.
Conclusion
Menopause is a unique life passage of changes that could occur, both physically and emotionally. That can be challenging, but the more informed a woman is with respect to what to expect and how to manage the symptoms, the easier the process becomes. With lifestyle adjustments and medical treatment or just being better informed, a woman becomes better equipped to handle menopause. Whatever concerns around menopause or its symptoms that may arise, never shy away from seeking advice and being supported by your health professional—always individually tailored to you.

by Womanaari | Aug 22, 2024 | Uncategorized
Understanding Rectocele: Causes, Symptoms, Diagnosis, and Treatment
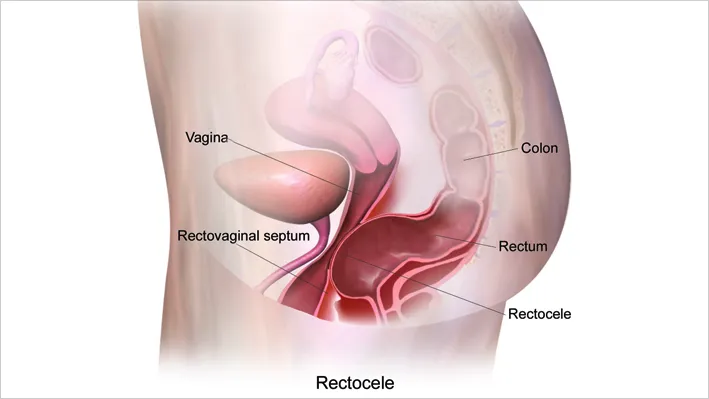
A rectocele is a condition that occurs when the thin wall of tissue between a woman’s rectum and vagina becomes weak, causing the rectum to bulge into the vaginal area. This can lead to discomfort and various symptoms, depending on the severity of the condition. While this may sound alarming, it’s important to note that a rectocele is treatable, and many women manage their symptoms effectively with medical or surgical interventions.
What Causes Rectocele?
The primary cause of a rectocele is prolonged pressure on the pelvic floor, which can weaken the muscles and tissues supporting the vagina and rectum. This pressure can come from several sources, including:
- Pregnancy and Childbirth: The physical strain of carrying a baby and the trauma of vaginal delivery can stretch and weaken the pelvic floor muscles, especially if there has been tearing or the need for an episiotomy (a surgical cut made at the opening of the vagina during childbirth).
- Aging: As women age, their muscles naturally lose strength and elasticity. This weakening includes the pelvic floor muscles, making older women more susceptible to developing a rectocele.
- Chronic Constipation: Constant straining to pass stool can put a great deal of pressure on the pelvic floor, contributing to the weakening of the tissue between the rectum and the vagina.
- Obesity: Carrying excess weight can increase pressure on the pelvic floor, leading to a higher risk of developing a rectocele.
- Chronic Cough or Bronchitis: Persistent coughing can repeatedly strain the pelvic floor muscles, similar to the effects of chronic constipation.
What Are the Symptoms of Rectocele?
The symptoms of a rectocele can vary widely depending on the size of the bulge and the severity of the condition. Some women with small rectoceles may not experience any symptoms at all and may only discover the condition during a routine pelvic examination. However, for those who do experience symptoms, they may include:
- Vaginal Pressure or Fullness: Many women report feeling a pressure or fullness inside the vagina, as if something is falling out. This sensation can be uncomfortable but is typically not painful.
- Difficulty with Bowel Movements: A rectocele can make it difficult to have a bowel movement. Some women may feel as though they have not completely emptied their rectum after using the bathroom. In some cases, women may need to manually support the back of the vaginal wall (a technique known as “splinting”) to help pass stool.
- Soft Bulge in the Vagina: A visible or palpable bulge of tissue may be noticeable inside the vagina or, in severe cases, protruding through the vaginal opening.
- Discomfort During Sexual Intercourse: The presence of a rectocele can lead to discomfort or a feeling of looseness during sex, which can be distressing for some women.
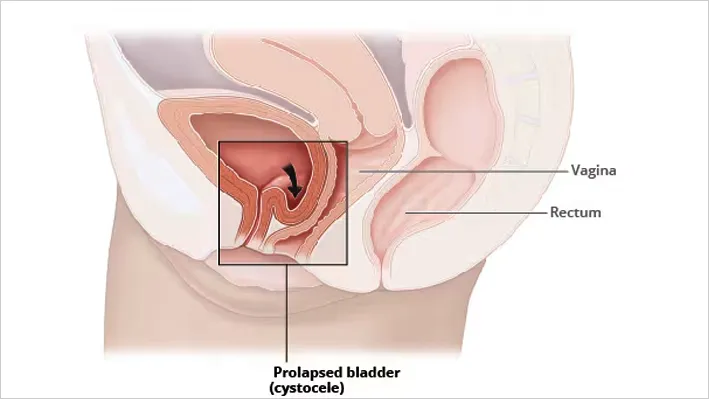
- Associated Pelvic Organ Prolapse: Women with a rectocele may also experience prolapse of other pelvic organs, such as the bladder (cystocele) or uterus (uterine prolapse), leading to additional symptoms like urinary incontinence.
How Is a Rectocele Diagnosed?
Diagnosis of a rectocele typically begins with a visit to a healthcare provider, who will take a detailed medical history and perform a physical examination. The doctor may visually inspect the pelvis and perform an internal exam to assess the extent of the rectocele. In most cases, this examination is sufficient to diagnose the condition.
In some cases, additional tests may be required to assess the overall health of the pelvic floor muscles or to identify other related conditions. These tests might include:
- Imaging Studies: Ultrasound or MRI may be used to get a clearer view of the pelvic organs and assess the function of the pelvic floor muscles.
- Endoanal Ultrasound or MRI Defecography: These specialized tests involve inserting gel into the rectum and vagina to visualize the pelvic organs during a bowel movement, helping to identify the severity of the rectocele and any other prolapses.
- Sigmoidoscopy or Colonoscopy: These procedures involve inserting a flexible tube with a camera into the rectum and colon to check for any abnormalities in the bowel that might be contributing to symptoms.
What Are the Treatment Options for Rectocele?
Treatment for rectocele varies based on the severity of symptoms and the impact on the woman’s quality of life. The options range from conservative, non-surgical approaches to surgical repair for more severe cases.
Medical Treatment Options:
- Dietary and Lifestyle Modifications: Increasing dietary fiber, using laxatives judiciously, and drinking plenty of fluids can help manage constipation, which in turn can reduce the strain on the pelvic floor. Women are also advised to avoid heavy lifting and excessive straining.
- Pelvic Floor Physical Therapy: Exercises like Kegels can strengthen the pelvic floor muscles and alleviate symptoms. Biofeedback therapy, guided by a physical therapist, can be particularly effective.
- Vaginal Pessary: This is a small plastic or rubber device inserted into the vagina to support the pelvic organs. It can be an effective non-surgical option, especially for older women or those with medical conditions that make surgery risky.
Surgical Treatment:
For women with significant symptoms that do not respond to conservative treatments, surgery may be necessary. The goal of surgery is to repair the weakened tissue, either through the vagina, rectum, or perineum. In some cases, tissue reinforcement with mesh may be used to provide additional support.
Conclusion
A rectocele is a common but often manageable condition. With proper diagnosis and treatment, most women can find relief from their symptoms and maintain a good quality of life. If you’re experiencing any of the symptoms mentioned, it’s important to seek medical advice to determine the best course of action for your specific situation.

by Womanaari | Aug 22, 2024 | Uncategorized
Uterine prolapse in Dubai is an issue that influences the pelvic floor muscles and ligaments that help the uterus. These muscles might get extended and frail and can prompt the uterus to descend or, regardless, stand out of the vagina. This condition is especially normal in ladies who have gone through menopause and have had at least one vaginal delivery.
Reasons for Uterine Prolapse Treatment in Dubai, UAE
The main cause of uterine prolapse is the weakening of the pelvic floor muscles and tendons. A few reasons can add to this debilitation:
1. Childbirth: One of the most generally perceived causes is the strain placed on the pelvic floor during labor. The more vaginal deliveries a woman has, the higher the possibility of having a prolapse she has in the future.
2. Maturing and Menopause: The release of the hormone called “estrogen” decreases when women get menopause. That hormone helps keep the pelvic muscles strong. The decrease in estrogen levels prompts weakening of these muscles.
3. Heavy Lifting and Stressing: Routinely lifting weighty items or stressing during bowel can put pressure on the pelvic floor, adding to its debilitating after some time.
4. Obesity: Having excess weight can strain the pelvic floor, making prolapse almost certain.
5. Chronic Coughing: Conditions that cause constant coughing, like smoking or persistent lung infections, can likewise expand the risk of prolapse because of the continuous burden on the pelvic floor muscles.
What if I don’t go for Uterine Prolapse Treatment?
This condition can influence different organs in the pelvic segment of your body. It relies on how serious the prolapse is. In gentle situations where your satisfaction isn’t impacted, your primary care physician probably won’t suggest any Uterine Prolapse Treatment in Dubai.
Side Effects of Uterine Prolapse
Numerous ladies with mild uterine prolapse in Dubai, UAE may not encounter any side effects. In any case, as the prolapse turns out to be more extreme, it can cause a scope of awkward and, once in a while, difficult side effects:
- A Sensation of Heaviness in the Pelvis: Numerous ladies depict having a feeling of weight or strain in the pelvic region, as though something is pulling down.
- Tissue Protruding from the Vagina: In additional serious cases, ladies might see tissue swelling out of the vaginal opening, which can be disturbing and awkward.
- Urinary Issues: Prolapse can prompt issues with pee, for example, trouble purging the bladder totally or encountering urinary incontinence (spilling pee).
- Gut Issues: A few ladies might experience difficulty with bowel movement, feeling like they need to push on the vagina to assist with passing stool.
- Distress during Sex: Sexual movement can become awkward or even difficult, and a few ladies feel like the vaginal tissue is free.
- Low Back Agony: The tension and strain from prolapse can likewise cause uneasiness in the lower back.
When should I Look for Clinical Assistance in Dubai?
If the side effects of uterine prolapse are causing distress or interrupting routine activities, looking for medical advice is essential. A medical services supplier in the UAE can evaluate the seriousness of the prolapse and examine the choice for Uterine Prolapse Treatment in Dubai for you.
How is Uterine Prolapse diagnosed in the UAE?
With a pelvic test, your clinician will check whether your uterus has dropped from its usual spot. A pelvic test is a normal test where your clinician puts a speculum-an instrument that permits them to glimpse inside your vagina-and looks inside your vagina and uterus outwardly. After the assessment, your clinician will tell you appropriately if you have been determined not to have uterine prolapse treatment choices.
Uterine Prolapse Treatment in the UAE
Here are some choices for Uterine Prolapse Treatment in Dubai that depend upon the seriousness of the condition and the lady’s overall health and lifestyle:
1. Lifestyle Changes and Activities: For mild prolapse, lifestyle changes like weight reduction, abstaining from difficult work, and overseeing ongoing coughing can assist with lessening side effects. Pelvic floor works out, known as Kegel worksout, can likewise reinforce the pelvic muscles and further develop support for the uterus.
2. Pessaries: A pessary is a device that is inserted inside the vagina to support the uterus and other pelvic organs. It comes in different shapes and sizes and can be a good choice for ladies who need to stay away from a medical procedure.
3. Minimally Obtrusive Medical procedure: In cases where the prolapse is more serious and side effects are affecting the life of the woman, a medical procedure might be vital. Insignificantly intrusive gynecologic medical procedures offer a few benefits over customary medical procedures.
4. Vaginal Hysterectomy: Some might be recommended removal of the uterus (hysterectomy) because of the seriousness of the condition. This should be possible through a negligibly obtrusive methodology, diminishing recuperation time.
5. Pelvic Floor Reconstruction: In additional complicated cases, a blend of careful methods might be utilized to re-form the pelvic floor and re-establish backing to the prolapsed organs.
What is the advantage of opting for a negligibly obtrusive medical procedure for uterine prolapse treatment in Dubai, UAE?
Minimally obtrusive medical procedure for uterine prolapse treatment offers a few advantages that include:
• Smaller Cuts and Less Scarring
• Less Torment
• Speedier Recuperation
• Lower Chance of Confusion
Even after Uterine Prolapse Treatment, Can uterine prolapse recur?
Most treatments for uterine prolapse are successful in Dubai. However, a prolapse can recur sometimes. This is more likely if you- have a very severe prolapse, have obesity or if, are younger than 60.
End
Uterine prolapse is a common condition in the UAE that influences numerous ladies. While the side effects can be awkward and now and again troubling, there are viable choices for Uterine Prolapse Treatment in Dubai accessible, going from way of life changes and activities to advanced insignificantly obtrusive medical procedures. On the off chance that you are encountering side effects of uterine prolapse, it is critical to talk with a medical care supplier in Dubai to examine the best option for your requirements.

by Womanaari | Aug 6, 2024 | Uncategorized
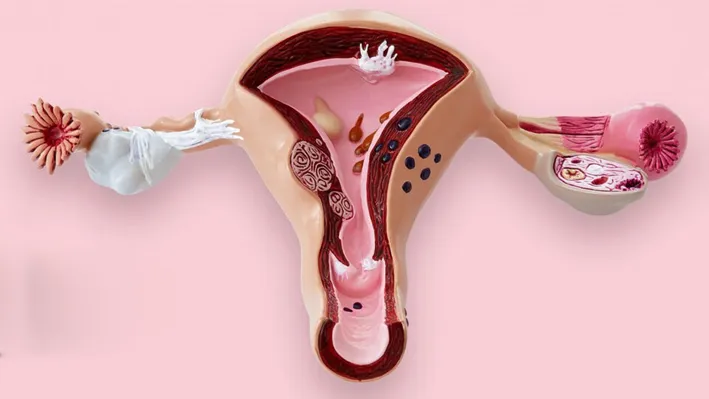
Uterine Prolapse Treatment also known as endometrial polyps, are growths in the Uterine cavith arising from the lining of the uterus ( endometrium)
They can vary in size, ranging from a few millimeters to several centimeters.
Uterine polyps are typically benign, though in rare cases, they can be precancerous or cancerous.
Common symptoms include irregular menstrual bleeding, heavy periods, bleeding between periods, or postmenopausal bleeding. Some women may also experience infertility or recurrent miscarriages due to the presence of polyps.
Risk factors for developing uterine polyps include age, particularly in women between 40 and 50, obesity, hypertension, and a history of hormone replacement therapy or tamoxifen use. Diagnosis is often achieved through ultrasound or Hysteroscopy.
Uterine prolapse treatment options include watchful waiting (if no symptoms) or surgical removal through hysteroscope depending on symptom severity and polyp characteristics.
This treatment offers viable relief from distress and pelvic strain. Surgical choices assist with re-establishing normal capability and work on personal satisfaction. By tending to the main cause, uterine prolapse treatment decreases side effects and prevents future complications, making it a fantastic decision for ladies looking for long-haul pelvic well-being.

by Womanaari | Aug 6, 2024 | Uncategorized
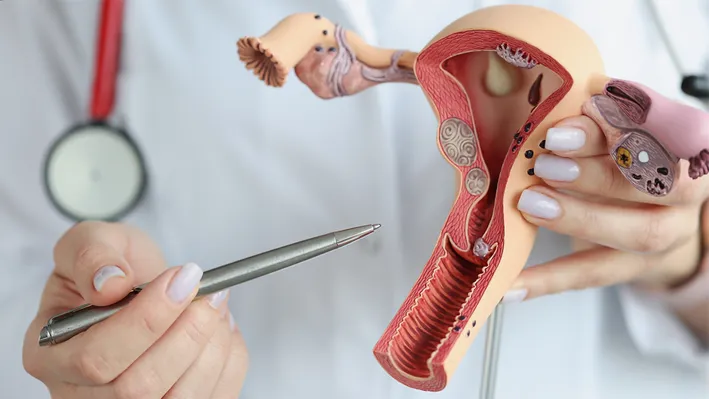
Hysterectomy is a surgical procedure that involves the removal of the uterus and, in some cases, the cervix, ovaries, and fallopian tubes. It is usually done in women over 40 years and who have finished childbearing unless for cancer it is done even in younger women who haven’t borne children.
Hysteroscopy and polyp removal is a common treatment for various gynecological conditions such as uterine fibroids, endometriosis, chronic pelvic pain, abnormal bleeding, and certain cancers.
There are different types of hysterectomy: total (removal of the uterus and cervix), subtotal or partial (removal of the uterus while leaving the cervix intact), and radical (removal of the uterus, cervix, parts of the vagina, and surrounding tissues, usually for cancer).
The hysteroscopy and polyp removal procedure can be performed through various surgical approaches, including abdominal, vaginal, or laparoscopic techniques.
The recent addition is the innovative vNOTES or scarless surgery.
The choice of method depends on the patient’s medical condition, the pathology for which it is being done, and the surgeon’s expertise.
Recovery time varies, with minimally invasive methods typically offering quicker recovery and less postoperative pain as compared to conventional open surgery.
A hysteroscopy and polyp removal can significantly improve the quality of life for women with debilitating symptoms, though it also results in the loss of fertility.

by Womanaari | Aug 6, 2024 | Uncategorized
Fibroids also known as uterine leiomyoma, are non-cancerous growths that develop in or around the uterus. They are composed of muscle and fibrous tissue and can vary greatly in size, from microscopic to as large as a melon. While the exact cause of fibroids is not well understood, factors such as genetics, hormones, and lifestyle may play a role. The majority of the time fibroids don’t cause any symptoms but when they are multiple and large in size can cause symptoms such as heavy menstrual bleeding, prolonged periods, pelvic pain and pressure, frequent urination, infertility, and complications during pregnancy.
The symptoms depend on their number, size, and location.
Based on their location they are classified as submucous, serosal, or intra-mural.
Treatment options range from monitoring with no treatment or medical management to control symptoms or dissolving them with non-invasive techniques such as MRI-guided focused ultrasound, Uterine artery embolisation, or surgical interventions such as endometriosis excision surgery.
The choice of treatment depends on factors like the severity of symptoms, the size and location of the fibroids, and the patient’s reproductive plans. However, opting for the surgery is a better option. Endometriosis excision surgery is a successful therapy for those experiencing constant pain and fertility issues brought about by endometriosis. By exactly eliminating endometrial tissue, this surgery offers long-haul relief, works on personal satisfaction, and better reproductive results. It is a strongly suggested choice for overseeing endometriosis side effects.
Laparoscopy in gynecology
Get Minimally Invasive Solutions Laparoscopy in Gynecology
Laparoscopy in gynecology is a minimally invasive surgical technique that uses a telescopic camera to visualize the internal organs in the pelvis and abdomen.
It helps surgeons to perform keyhole surgery with small 0.5 to 1cm skin incisions to diagnose and treat various gynecological conditions such as infertility, fibroids, endometriosis, pelvic pain, ovarian cysts, and many more including cancer.
All surgeries which were previously performed as an open procedure with big skin incisions are now performed laparoscopically. Some of the commonly performed surgeries in gynecology through a laparoscope are Laparoscopic myomectomy (removal of fibroid), ovarian cystectomy, hysterectomy (removal of the uterus), salpingectomy (removal of the fallopian tube), excision of endometriosis, treatment of ectopic pregnancy, etc.
The advantages of Laparoscopy in gynecology include reduced postoperative pain, shorter hospital stays, faster recovery times, and minimal scarring compared to traditional open surgery.
Additionally, this method lowers the risk of complications and infections, enhancing patient safety and comfort.
As medical technology advances, Laparoscopy in gynecology continues to evolve, providing women with more effective and less invasive surgical options.
Myomectomy ( removal of fibroids or myoma)
Effective Removal of Fibroids Myomectomy
Myomectomy ( removal of fibroids or myoma) is a surgical procedure for removing uterine fibroids while preserving the uterus. It is often chosen by women who wish to retain their fertility or uterus.
A myomectomy can be performed
1. Through a conventional abdominal cut either (open procedure)
2. laparoscopically as a keyhole surgery
3. hysteroscopic surgery if the myoma (fibroid) is entirely inside the Uterine cavity (submucous)
4. VNOTES (scarless surgery) which uses a telescope through the vagina.
The approach is decided based on the size, number, and location of the fibroids.
Abdominal myomectomy involves a larger incision in the abdomen, whereas laparoscopic and hysteroscopic myomectomies are minimally invasive, utilizing small incisions and specialized instruments.
Myomectomy ( removal of fibroids or myoma) surgery can alleviate symptoms such as heavy menstrual bleeding, pelvic pain, and pressure on the bladder or bowel. Recovery times vary based on the surgical approach, with minimally invasive techniques generally offering faster recovery and less postoperative pain.
Myomectomy provides symptomatic relief and improves the quality of life for many women while preserving their reproductive potential.