Understanding Rectocele: Causes, Symptoms, Diagnosis, and Treatment
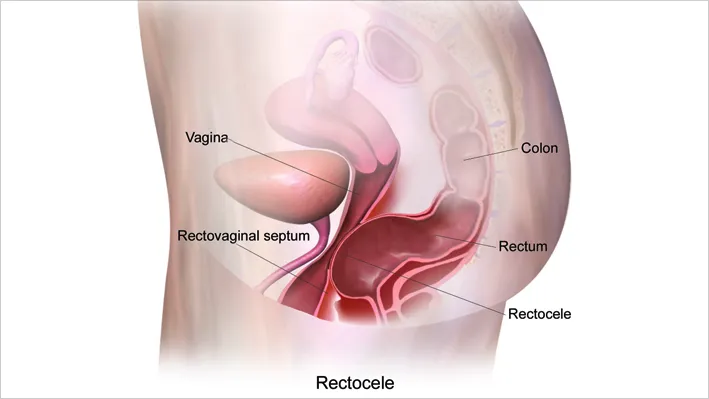
A rectocele is a condition that occurs when the thin wall of tissue between a woman’s rectum and vagina becomes weak, causing the rectum to bulge into the vaginal area. This can lead to discomfort and various symptoms, depending on the severity of the condition. While this may sound alarming, it’s important to note that a rectocele is treatable, and many women manage their symptoms effectively with medical or surgical interventions.
What Causes Rectocele?
The primary cause of a rectocele is prolonged pressure on the pelvic floor, which can weaken the muscles and tissues supporting the vagina and rectum. This pressure can come from several sources, including:
- Pregnancy and Childbirth: The physical strain of carrying a baby and the trauma of vaginal delivery can stretch and weaken the pelvic floor muscles, especially if there has been tearing or the need for an episiotomy (a surgical cut made at the opening of the vagina during childbirth).
- Aging: As women age, their muscles naturally lose strength and elasticity. This weakening includes the pelvic floor muscles, making older women more susceptible to developing a rectocele.
- Chronic Constipation: Constant straining to pass stool can put a great deal of pressure on the pelvic floor, contributing to the weakening of the tissue between the rectum and the vagina.
- Obesity: Carrying excess weight can increase pressure on the pelvic floor, leading to a higher risk of developing a rectocele.
- Chronic Cough or Bronchitis: Persistent coughing can repeatedly strain the pelvic floor muscles, similar to the effects of chronic constipation.
What Are the Symptoms of Rectocele?
The symptoms of a rectocele can vary widely depending on the size of the bulge and the severity of the condition. Some women with small rectoceles may not experience any symptoms at all and may only discover the condition during a routine pelvic examination. However, for those who do experience symptoms, they may include:
- Vaginal Pressure or Fullness: Many women report feeling a pressure or fullness inside the vagina, as if something is falling out. This sensation can be uncomfortable but is typically not painful.
- Difficulty with Bowel Movements: A rectocele can make it difficult to have a bowel movement. Some women may feel as though they have not completely emptied their rectum after using the bathroom. In some cases, women may need to manually support the back of the vaginal wall (a technique known as “splinting”) to help pass stool.
- Soft Bulge in the Vagina: A visible or palpable bulge of tissue may be noticeable inside the vagina or, in severe cases, protruding through the vaginal opening.
- Discomfort During Sexual Intercourse: The presence of a rectocele can lead to discomfort or a feeling of looseness during sex, which can be distressing for some women.
- Associated Pelvic Organ Prolapse: Women with a rectocele may also experience prolapse of other pelvic organs, such as the bladder (cystocele) or uterus (uterine prolapse), leading to additional symptoms like urinary incontinence.
How Is a Rectocele Diagnosed?
Diagnosis of a rectocele typically begins with a visit to a healthcare provider, who will take a detailed medical history and perform a physical examination. The doctor may visually inspect the pelvis and perform an internal exam to assess the extent of the rectocele. In most cases, this examination is sufficient to diagnose the condition.
In some cases, additional tests may be required to assess the overall health of the pelvic floor muscles or to identify other related conditions. These tests might include:
- Imaging Studies: Ultrasound or MRI may be used to get a clearer view of the pelvic organs and assess the function of the pelvic floor muscles.
- Endoanal Ultrasound or MRI Defecography: These specialized tests involve inserting gel into the rectum and vagina to visualize the pelvic organs during a bowel movement, helping to identify the severity of the rectocele and any other prolapses.
- Sigmoidoscopy or Colonoscopy: These procedures involve inserting a flexible tube with a camera into the rectum and colon to check for any abnormalities in the bowel that might be contributing to symptoms.
What Are the Treatment Options for Rectocele?
Treatment for rectocele varies based on the severity of symptoms and the impact on the woman’s quality of life. The options range from conservative, non-surgical approaches to surgical repair for more severe cases.
Medical Treatment Options:
- Dietary and Lifestyle Modifications: Increasing dietary fiber, using laxatives judiciously, and drinking plenty of fluids can help manage constipation, which in turn can reduce the strain on the pelvic floor. Women are also advised to avoid heavy lifting and excessive straining.
- Pelvic Floor Physical Therapy: Exercises like Kegels can strengthen the pelvic floor muscles and alleviate symptoms. Biofeedback therapy, guided by a physical therapist, can be particularly effective.
- Vaginal Pessary: This is a small plastic or rubber device inserted into the vagina to support the pelvic organs. It can be an effective non-surgical option, especially for older women or those with medical conditions that make surgery risky.
Surgical Treatment:
For women with significant symptoms that do not respond to conservative treatments, surgery may be necessary. The goal of surgery is to repair the weakened tissue, either through the vagina, rectum, or perineum. In some cases, tissue reinforcement with mesh may be used to provide additional support.
Conclusion
A rectocele is a common but often manageable condition. With proper diagnosis and treatment, most women can find relief from their symptoms and maintain a good quality of life. If you’re experiencing any of the symptoms mentioned, it’s important to seek medical advice to determine the best course of action for your specific situation.



0 Comments